INTRODUCTION
In 2021, the estimated number of people diagnosed with tuberculosis (TB) increased by 4.5%, mainly due to the disruption of TB services caused by the COVD-19 pandemic leading to delayed diagnosis and treatment initiation. Although specific data regarding extrapulmonary (EPTB) incidence are not available, it is estimated that EPTB accounts for approximately 15–25% of TB infections1. Head and neck TB (HNTB) represents 10% of EPTB cases and mainly affects the cervical lymph nodes, larynx, middle ear, oral cavity and pharynx2,3. More specifically, ΤΒ affecting the orofacial region is very rare affecting only 0.1–5% of extrapulmonary TB cases4.
Involvement of the temporomandibular joint (TMJ) is extremely rare, with only a few cases reported in the literature. As a matter of fact, TMJ TB accounts for <2% of skeletal TB sites5.
Unfortunately, symptoms usually appear at an advanced stage and include mainly preauricular swelling, trismus (difficulty in mouth opening) and joint stiffness6. The main abnormality is formation of an abscess along with varying degrees of bone destruction, which can result even in the formation of a fistula4,.
Simple imaging studies such as panoramic dental X-rays, show the osteolytic lesion or lysis and condensation usually with fuzzy limits. CT scans provide a more detailed illustration of the abnormalities, including periodontitis with bone loss, bone remodeling with osteolysis and osteo condensation, and pre-mandibular soft tissue abscess7. MRI may be more effective in detecting TB abnormalities in peripheral joints. Even though the presence of pus either on CT or MRI is not always apparent, the presence of fluid favors a diagnosis of TMJ TB8.
The infection begins in the subchondral region and progresses to affect the cartilage, synovium and joint space. The cancellous portion of the mandibular condyle is particularly susceptible to TB, since this part of the bone is affected in the beginning4.
TMJ TB accounts for an osteoarticular TB form as it usually involves the cancellous portion of the mandibular condyle. M. tuberculosis inoculates there by hematogenous dissemination4. Nevertheless, TMJ TB can be a complicated manifestation of TB of the oral cavity. Oral TB, although uncommon due to natural defensive mechanisms, can involve the buccal mucosa, tongue, gingiva, and mandible9. Interestingly, in an older review concerning TB of the oral cavity, it was reported that the second most commonly affected area was the mandible (21.4%)10. Mandibular osteomyelitis presents with signs of atypical osteitis, periodontal disease with vertical bone loss, or destructive osteolysis. Discharge of pus or blood was described either by sinuses, tooth sockets, even by the spicules of bones through the gums10. It appears that abnormalities follow gradual involvement of adjacent tissues but it is not known which is the primary site of infection; the mandible or is it the oral cavity? The latter can be explained as it is known that breaks in the continuity of the mucosa, such as trauma, allow invasion of M. tuberculosis into deeper tissues, including the facial bones9. Local factors that may facilitate invasion of the oral mucosa include poor oral hygiene, leukoplakia, local trauma, and irritation by clove chewing11. Interestingly, TMJ TB has even been reported to arise from a fistulous communication from the middle ear12.
Diagnosing TMJ TB requires confirming the presence of M. tuberculosis through microbiological tests such as AFB, molecular or culture, either by bone biopsy or more commonly via a fine needle aspiration of the pus. While TMJ TB can rarely present as a primary form of TB4, it is more commonly associated with pulmonary disease. When a patient presents with both pulmonary TB and TMJ abnormalities, it is highly likely that TMJ TB is also present. In this case, a good response to treatment, both clinically and based on imaging findings is expected.
Differential diagnosis for TMJ TB includes other conditions like abscess, arthritis, osteomyelitis, neoplasmatic disease, or any systemic diseases that affect the joints. Pathology of the surrounding structures, e.g. teeth and the parotid gland, have to be ruled out.
Treatment of TMJ TB is similar to that of pulmonary TB, although it requires a significant amount of time, typically 6–9 months or even longer. The presence of other affected organs from tuberculosis also determines the final regimen. In our case, which is the first reported to have concomitant pulmonary and CNS tuberculosis, a high dose of rifampicin was used (900 mg), given new data. Moreover, since M. tuberculosis was sensitive to all first-class medicines a quinolone was added to increase treatment efficacy regarding CNS involvement. The extent of TMJ destruction at the time of diagnosis and treatment initiation determines the level of functionality afterwards. Early diagnosis is crucial for achieving the best possible quality of life. In fact, around 90–95% of TMJ TB patients regain normal masticatory function, when treatment is initiated at an early stage13. Surgical interventions such as decortications and excision are only considered when oral drug treatment seems insufficient4. The treatment of orofacial TB varies, depending on its presentation. According to the literature, cases with minimal destructive lesions typically respond to medical intervention with anti-tubercular therapy, leading to resolution, without the need for surgical treatment. On the other hand, moderately destructive lesions may necessitate decortication of bone due to medullary bone destruction and/or cortical bone perforation14.
CASE PRESENTATION
A 20-year-old female patient of African origin presented to the hospital with pain in the mandible, swelling at the left masticator and inability of complete mouth opening since one month ago. The patient was admitted to the internal medicine department for further investigation and treatment.
The patient had no significant medical history, except for a tooth extraction 3 years ago, and was not taking any medications. She was afebrile, and all her vital signs were within the normal range. Swelling and pain at palpation were observed upon palpation of the left temporomandibular joint and the masticator muscle area. Additionally, the patient had proptosis (exophthalmos) in her right eye without experiencing diplopia. She mentioned a non-productive cough over the past month. Neurologic examination revealed no deficits.
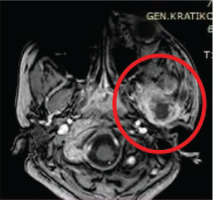
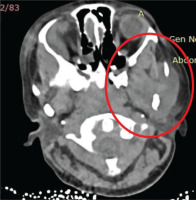
The patient underwent a chest and brain CT scan which revealed multiple hyperdense lesions in the right frontal and temporal lobe with peripheral enhancement and surrounding swelling. The largest lesion was 1.6 cm in the frontal lobe (Figure 1). Leptomeningeal enhancement was also observed. These findings were consistent with multiple abscesses and meningitis. Moreover, severe impairment and the presence of an abscess were observed in the right parietal bone. The tuber of the left mandible, the mandible itself, as well as the left masseter muscle appeared to be affected (Figures 2 and 3). Fluid consistent with an abscess was also present at the area. Since MRI is more sensitive than CT scanning in determining the extent of meningeal and parenchymal involvement, an MRI was performed and confirmed all the aforementioned lesions. Chest CT scan revealed centrilobular nodules and traction bronchiectasis in both upper lung lobes.
Figure 1
CT brain: hyperdense lesion in the right frontal lobe (1.6 cm) with peripheral enhancement and surrounding swelling

Figure 2
CT brain: destruction of the tuber of the left mandible, the temporal bone and edema of the left masseter muscle
Laboratory tests showed elevated inflammatory markers (CRP, ESR). The patient tested negative for HIV, HCV and HBV, while the Quantiferon test was positive.
Initially, the patient received common antibiotics with ceftriaxone and vancomycin but showed no improvement. Therefore, surgical drainage of the mandibular abscess was performed. The drained fluid was examined for common bacteria, fungus, toxoplasma, nocardia and mycobacteria. The AFB smear and the molecular test (XPERT MTB/RIF) were positive for M. tuberculosis. The detected strain was sensitive to rifampicin.
The patient was treated with isoniazid, high dose rifampicin (900 mg), pyrazinamide, ethambutol, and moxifloxacin. Current data support the use of higher doses of rifampicin (i.e. 35 mg/kg) in order to achieve increased CNS penetration. The use of levofloxacin instead of moxifloxacin is preferable due to reduced levels of the latter when co-administered with rifampicin. However, the patient presented an allergic reaction to levofloxacin, and moxifloxacin was administered instead. The patient responded well to the treatment both clinically and radiologically, in terms of CT findings.
During hospitalization, the patient experienced an episode of generalized tonic-clonic convulsions, resulting in a traumatic fracture of the cervical vertebrae A2. A brain CT scan was repeated and revealed further damage of the odontoid process of the A2 vertebrae. The patient was started on daily anticonvulsant treatment (levetiracetam) and no further seizures occurred.
The patient was discharged from the hospital after 34 days and continued follow-up at the Antituberculous Department of the Chest Disease Hospital. She received treatment for another 12 months and improved significantly. Follow-up CT scans showed improvement or remission of most lesions in both the brain and chest.
DISCUSSION
Diagnosis of TMJ TB can be challenging, especially when it presents as the primary symptom. Delayed diagnosis may be observed due to a lack of strong suspicion. Patients often lack pathognomonic signs, and exhibit fewer systemic symptoms, and even the typical tests performed when TB is suspected such as Tuberculin Skin Test (TST) yield positive results in only about half of the patients (53%)14. Unlike pulmonary TB, only 20% of head and neck TB patients experience typical symptoms such as cough, fever, or night sweats14. An overview of relevant studies of cases of TB infections of the TMJ is given in Table 1.
Table 1
Overview of cases of TB infections of the TMJ
| Authors | Age | Gender | Symptoms/clinical findings | Imaging findings | Type of operation | Other sites of TB co-infection | Type and duration of treatment |
|---|---|---|---|---|---|---|---|
| Geetha et al.4 | 49 | Female | Swelling in front of the left tragus | Destruction of the left mandibular condyle with proximal sclerosis and erosion of mandibular foss | Condylectomy | None | 6 months standard regimen |
| Helbling et al.6 | 22 | Female | Swelling and pain in the left preauricular area | Destruction of the left condyle and condylar fossa | FNA | None | 9 months standard regimen |
| Park et al.8 | 53 | Male | Painful swelling in the right preauricular area + difficulty in mouth opening since 3 months | Destructive changes of the right condyle glenoid fossa and ring enhancement of the preauricular area of the TMJ | Incision and drainage | Lumbar spondylodiscitis | 6 months standard regimen |
| Mohad et al.15 | 12 | Male | Swelling in the right preauricular area and difficulty in mouth opening since 2 months | Pronounced rarefaction and destruction of bone in mandibular condyle with discontinuity of the cortical boundary | FNA + incision | None | Unknown duration, standard regimen |
| Sheikh et al.16 | 20 | Male | Swelling in the right preauricular area | Erosion with comminuted destruction of the right mandibular condyle + abscess | Us guided FNA | Bilateral paravertebral and prevertebral abscess at L5– S1 level + right sacroiliac joint | 9 months standard regimen |
| Kumar et al.17 | 35 | Male | Swelling in the left preauricular area + difficulty in mouth opening | Erosion with the trabecular destruction of the left mandibular condyle + abscess+ cervical lymphadenopathy | FNA | None | INH/RIF for 9 months + condylectomy |
| Koul et al.18 | 16 | Female | Left-sided preauricular facial swelling + trismus | Rarefaction + destruction of bone with a large mass in retromandibular and inferior temporal fossa | Trucut biopsy | None | 9 months standard regimen |
| Karjodkar et al.19 | A 18 | Female | Swelling on left preauricular region + trismus since 8 months | Osteomyelitic changes in relation to left condyle and ramus | FNA | None | NA |
| B 45 | Male | Swelling on right side at the angle of the jaw since 2 months + teeth extraction due to pain | Irregular destruction at the angle region + osteomyelitis of the mandible | FNA | None | NA |
CONCLUSION
This case presentation emphasizes the importance of considering TB as part of the differential diagnosis, particularly for patients from endemic areas. In such cases investigation for lung involvement reinforces the diagnosis. Regrettably, there is a growing necessity to report and record each case of extrapulmonary TB, in order to guide the diagnostic approach for uncommon sites of infection.