INTRODUCTION
Cough is an important protective reflex in adults. It is an innate immunity mechanism that clears the airways from mucus, noxious agents, and pathogens. Cough represents a common symptom for medical assessment mainly in the primary care setting. In a retrospective study of 200000 patients in the UK, approximately 18% of the total population was assessed by a primary health care physician for a condition related to cough, acute or chronic1. A metaanalysis of 90 studies showed that the overall prevalence of chronic cough was 9.6% worldwide, with higher rates in Oceania (18.1%), Europe (12.7%) and America (11%) compared to Asia (4.4%) and Africa (2.3%)2. Another study of 10032 patients in specialized cough clinics showed that chronic cough was more common in females aged between the 5th and 7th decade3. Chronic cough is reported by patients at a rate ranging from 10% to 38% 4. It is more common in smokers and is related to environmental conditions as its prevalence increases with the mean annual concentration of nitrogen dioxide, total suspended particulates and particulates less than 10 μm in diameter in the atmosphere5. Several population studies have shown an increase in the prevalence of chronic cough worldwide due to increase in conditions and diseases such as bronchiectasis, asthma, GERD, upper airway cough syndrome, low income, smoking, occupation exposure to dust/fumes, low vegetable intake and abdominal obesity6.
CHALLENGES OF COUGH IN ADULTS
Physiology and complications of cough
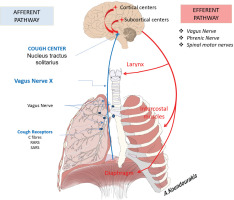
Cough represents a defense mechanism through which the human body removes redundant sputum and any irritants from the airways. It is the manifestation of a complex reflex that starts with the stimulation of receptors that activate the afferent (ascending) pathway and is associated with the following nerves: 1) vagus nerve and its branches in pharynx, upper larynx, and stomach; 2) glossopharyngeal nerve; 3) phrenic nerve; and 4) trigeminal nerve. Afferent nerves transfer signals to the center of cough which is located in the medulla oblongata. Central mechanisms (cortical and subcortical centers) allow for voluntary modulation of cough through down regulation of brainstem processing7. Efferent signals are transferred to the expiratory muscles through specific nerves, such as the phrenic nerve to the diaphragm and spinal motor nerves for the intercostal muscles (Figure 1).
Cough can be a significant factor in the spread of respiratory infections (such as SARS-CoV-2, influenza, streptococcal infection, etc.). Intense cough may result in numerous complications, such as hoarseness, urinary incontinence, syncope, vomiting, musculoskeletal pain and fractures, hernias, sleep disorders, headache, exhaustion, relationship problems, significant psychological consequences (50% of patients in cough clinics meet the criteria for depression) and traffic accidents8.
Evaluation of cough in outpatient clinics/primary care
The patient’s medical history provides the most significant information when assessing a patient with cough. It should include details on symptoms, previous diseases and medications, as well as the main characteristics of cough.
The onset and the duration of cough will determine whether cough is acute, subacute, or chronic and will guide us to corresponding causes and their investigation. Further determinants for cough evaluation involve the presence of sputum, previous episodes of cough, daily fluctuations, possible triggering causes, seasonal variations, association with meals, smoking, specific medications, atopy, travel abroad and the patient’s country of origin (e.g. areas endemic for tuberculosis, TBC) but also other systemic manifestations such as fever, sweating and weight loss.
The severity of cough can be assessed by three elements: its daily frequency and possible fluctuations, its intensity and finally how much it impacts the patient’s daily activities or sleep. For the accurate assessment of the severity of the cough, several useful tools have been designed such as visual analogue scale (VAS) and the cough symptom score (CSS). In clinical practice, VAS scales are preferred and are widely used for the subjective assessment and long-term evaluation (response to treatment, etc.) of cough (Figure 2)9. To assess the impact of cough on the patient’s quality of life (health-related quality of life, HRQOL) questionnaires can be used such as the Cough-specific Quality-of-Life Questionnaire (CQLQ), the Leicester Cough Questionnaire (LCQ) and the St George’s Respiratory Questionnaire (SGRQ)10. An important tool for assessing gastroesophageal reflux as a possible cause of cough is the Hull Cough Hypersensitivity Questionnaire available on the Hull Cough Hypersensitivity Questionnaire website (www.issc.info).
Etiology of cough
Cough can often be the main symptom of numerous lung-related and other diseases. The initial step in narrowing down the list of potential diagnoses and guiding the subsequent investigation is to determine the duration of cough. For adult patients complaining of cough, acute cough is defined as being less than 3 weeks in duration, subacute cough is defined as being between 3 and 8 weeks in duration and chronic cough is defined as being more than 8 weeks in duration11,12. The most frequent causes of cough, categorized by its duration, are presented in Table 1.
Table 1
The most frequent causes of a cough, categorized by its duration
Evaluation of acute cough
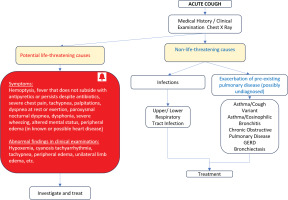
For the differential diagnosis of acute cough (duration less than 3 weeks) a detailed medical history and thorough clinical examination often lead to an initial diagnosis.
What needs to be assessed first are the characteristics of cough (productive or dry, intensity, duration and frequency) as well as any other symptoms such as fever and shortness of breath (dyspnea). VAS and quality of life questionnaires may help the clinician evaluate the characteristics of cough. A detailed medical history must also include information on the residence and living conditions of the patient, recent travel abroad, occupational or environmental exposure, and contact with people with respiratory infection. Acute cough could also be a symptom of exacerbation of pre-existing conditions such as asthma and COPD. Acute cough may also be the initial presentation of all diseases that cause chronic cough.
When assessing a patient with acute cough it is of major importance to exclude all potential life-threatening causes, such as foreign body aspiration, severe pneumonia, severe COPD exacerbation, pulmonary embolism, cardiac diseases, and many others. Alarming symptoms and clinical findings (red bell) suggestive of potential life-threatening diseases are described in the red table of Algorithm 1 and need prompt intervention.
When high risk conditions are excluded, the clinician must differentiate other, non-life-threatening, diseases13. The most common causes are mild infections, mainly viral, of the upper and lower respiratory tract. Subsequently, it is recommended to examine as a possible cause of acute cough the exacerbation of a pre-existing condition such as asthma, COPD (diseases that may be undiagnosed), upper airway cough syndrome (previously known as postnasal drip), bronchiectasis, etc. Potential occupational or environmental causes must also be recognized, so that the patient can avoid exposure to them.
The choice of the appropriate diagnostic tools for the assessment of acute cough is up to the doctor, based on medical history and clinical examination.
For the assessment of acute cough Algorithm 1 is suggested (Figure 3). The most common causes of acute cough are listed in Table 2.
Table 2
The most common causes of acute cough (duration ≤3 weeks)
Evaluation of subacute cough
Subacute cough (duration 3–8 weeks) is usually post infectious, presenting mainly after viral infections of the upper airway system. Similarly to acute cough, any cause of chronic cough should be taken into consideration at the differential diagnosis of the subacute cough. The most common causes are listed in Table 3.
Table 3
The most common causes of subacute cough (duration 3–8 weeks)
| Post infectious |
| Non-post infectious Acute exacerbation of a chronic disease of the lungs (preexisting or new onset) |
After excluding potential life-threatening conditions (red bell symptoms/findings), it is suggested to investigate the possible correlation of subacute cough with a recent history of infectious disease (Algorithm 2, Figure 4), as several pulmonary infectious diseases can cause cough with a duration of more than 3 weeks12. The clinician should check that the cough gradually improves with time and that the patient has received the appropriate treatment. For the treatment of post-infectious cough empirical therapy with bronchodilation or antitussives could be prescribed, without a proven benefit in clinical trials14.
Figure 4
Algorithm 2: Investigation of subacute cough (duration 3–8 weeks) (GERD, gastroesophageal reflux disease)
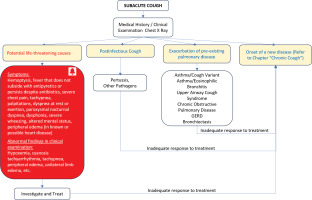
The presence of severe episodes of cough, followed by vomiting and/or syncope could lead to the diagnosis of pertussis, especially in young adults or children caregivers15. Patients with pertussis present with intermittent cough and possibly low-grade fever the first two weeks of illness, and cough persists up to 8 weeks. The diagnosis is made using B. Pertussis nasopharyngeal specimen culture (specificity 100% and sensitivity between 15–45%) or PCR (specificity 100%, sensitivity 65–97%). Culture is time consuming, and PCR is expensive and not widely used. For these reasons treatment with azithromycin or clarithromycin and assessment of the clinical outcome, is suggested.
Evaluation of chronic cough
The initial step for the investigation of chronic cough is the detailed history. What needs to be assessed are the characteristics of cough (wet, dry, intensity, duration, frequency, fluctuations, and possible triggering causes), patient’s smoking habit, current diseases and use of medications that can cause cough. Clinical examination is also the cornerstone of the diagnosis of chronic cough. Findings such as wheezing, diminished respiratory sounds, bilateral velcro sounds, clubbing, peripheral edema etc., can often lead to a possible diagnosis, narrowing the differential diagnosis tests. In most cases of patients with chronic cough we suggest imaging with a simple chest X-ray. The most common causes of chronic cough based on X-ray findings are mentioned in Table 4.
Table 4
The most common causes of chronic cough based on X-ray findings (*may present with normal chest X-ray)
A detailed algorithm for chronic cough is provided (Algorithm 3, Figure 5). What needs to be excluded first, are life-threatening conditions when specific symptoms and clinical signs (red bell symptoms/findings) exist. Once they are excluded, the clinician must investigate other, non-lifethreatening diseases, driven by initial clinical and laboratory findings. Iatrogenic cough (medications) and smoking are also other common causes of cough that can be possibly diagnosed only by medical history.
Figure 5
Algorithm 3: Chronic cough investigation (ACE, angiotensin-converting enzyme inhibitors; HRCT, high resolution computerized tomography; ECG, electrocardiogram; ECHO, echocardiogram)
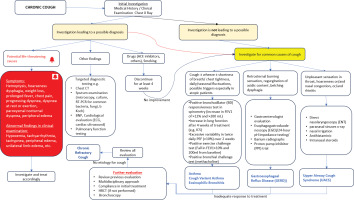
When the findings from initial investigation do not lead to a possible diagnosis for chronic cough, the most common causes of chronic cough should be investigated. These are upper airway cough syndrome (UACS), asthma (including cough variant asthma), eosinophilic bronchitis, and gastroesophageal reflux (GERD)12.
When the investigation does not lead to a diagnosis and all possible therapeutic trials fail, the patient must be re-evaluated using a multidisciplinary approach. Further testing (e.g. HRCT if not performed or bronchoscopy) may also be necessary. When cough persists despite guideline-based treatment, the patient may suffer from chronic refractory cough (CRC).
Common causes of chronic cough
Asthma
Bronchial asthma is one of the most common causes of chronic cough. The diagnosis of asthma is based on identifying both characteristic patterns of respiratory symptoms such as wheezing, shortness of breath (dyspnea), chest tightness or cough, and variable expiratory airflow limitation. Flow variability is usually confirmed by positive bronchodilator (BD) responsiveness test in spirometry (increase in FEV1 of >12% and >200 mL). Other evidence is increase in lung function after 4 weeks of treatment (e.g. ICS), excessive variability in twice daily PEF (>10%) over 2 weeks and positive exercise challenge test (fall in FEV1>10% and 200 mL from baseline)16. Further investigation of bronchial hyper-responsiveness with positive bronchial challenge test (methacholine or histamine) has a high negative predictive value, but it is difficult to perform especially in primary care settings.
Confirmation of eosinophilic inflammation [sputum cell count, fractional exhaled nitric oxide (FENO), blood eosinophils etc.] may be a useful biomarker in chronic asthmatic cough, for both diagnosis and treatment selection17.
Cough-variant asthma (CVA)
Cough variant asthma is a term which describes asthmatic patients with normal lung function tests and chronic cough, as the only symptom, that improves after the administration of bronchodilators18. Treatment similar to that of asthma is recommended and response to treatment is evaluated after 4 weeks19. Patients with suspected CVA may also be given a trial of oral steroids for one week. Although published guidelines do not specify a recommended dose, 40 mg of prednisolone equivalent is usually used. This approach may positively impact cough20.
Eosinophilic bronchitis
Eosinophilic (non-asthmatic) bronchitis is the condition in which there is a chronic cough and proven eosinophilic inflammation of the airways, without expiratory flow limitation (obstructive spirometry or flow measurement variation) and without hyper-reactivity21. Based on data from observational studies, a treatment similar to that of asthma is recommended. Since asthma, cough-variant asthma and non-asthmatic eosinophilic bronchitis respond to ICS treatment, it is recommended that these 3 entities are included in the asthma spectrum when addressing the primary care patient.
Gastroesophageal reflux disease
The most typical symptoms of GERD are retrosternal burning sensation, acid reflux and regurgitation, which are exacerbated after meals and during morning arousal, and are typically absent at night22. Other symptoms, such as dysphonia, dysgeusia, chronic nasal congestion and/or a runny nose, are explained by reflux and subsequent microaspiration of acidic gastric fluid into the bronchial tree23. A possible mechanism of cough at GERD is the direct stimulation of gastric content (acidic, non-acidic or even aerated) to the lower afferent fibers of the esophagus, larynx or tracheobronchial tree, and the inflammation that is caused by the ingested material24.
In the absence of typical GERD symptoms, it is not recommended to screen patients with chronic cough for GERD. Treatment with antisecretory therapy (H2-receptor blockers, H2-agonists and proton pump inhibitors PPIs) is only recommended when symptoms compatible with gastritis or GERD are present, as the benefit in reducing cough is modest and response rates are low (approximately 28%)25. A trial of proton pump inhibitors for one month at the standard dose, twice daily, 30–60 min before meals is recommended26. H2-receptor blockers can be administered as an add-on therapy to proton pump inhibitors although evidence is poor27. Eukinetics, such as metoclopramide, domperidone and azithromycin that promote intestinal motility, are not recommended for the treatment of chronic cough. Standard conservative interventions to reduce reflux are important, such as weight loss, night-time bed rest with the head in a higher than horizontal position and dietary measures (food intake avoidance before bedtime, restriction of acidic, fatty and spicy foods, and sugary drinks).
In patients with chronic cough and typical GERD symptoms who do respond to high doses of PPIs, further diagnostic testing should be performed by a specialist gastroenterologist, including upper gastrointestinal endoscopy, 24-hour esophageal pH recording, barium esophagography, and esophageal manometry.
Upper airway cough syndrome
Upper airway cough syndrome (UACS) includes many conditions, such as post-nasal drip syndrome (a term that tends to be abandoned), allergic and non-allergic rhinitis, vasomotor rhinitis, and chronic rhinosinusitis, with or without nasal polyposis28. Suspicion of this syndrome is raised when a patient describes a feeling of a foreign body in the throat, ‘like something dripping down the throat’ or a need to ‘clear the throat’, gagging, and/or nasal congestion, and/or catarrh29. Clinical examination of the nasopharynx and oropharynx may reveal the presence of mucous or mucopurulent discharge. Endoscopic examination of the upper respiratory tract may reveal redness and swelling of the larynx.
Esophageal dyskinesia is classified as a separate condition under the name esophagopharyngeal-pharyngeal or laryngeal-pharyngeal reflux30. Esophageal dyskinesia is detected with barium esophagography, but due to its low sensitivity esophageal manometry is recommended12,31.
Induced laryngeal obstruction manifests with vocal cord dysfunction, dyspnea, and cough-induced speech interruption. It is attributed to the hyper-responsiveness of the larynx and is detected during endoscopic examination when closure of the vocal cords is observed during the inhalation effort. It does not respond to medical treatment and is treated with speech therapy32.
Endoscopic upper respiratory tract examination and cranial computed tomography scanning are not recommended as routine tests in all patients with chronic cough12.
Pharmacological management of UACS is empirical, including nasal washings and intranasal corticosteroids (from 2 to 8 weeks), nasal decongestants and firstgeneration antihistamines14. First-generation antihistamines contribute to cough remission through central activity as anticholinergics. Second-generation antihistamines are not as effective as first-generation antihistamines in the treatment of chronic cough33.
Iatrogenic cough (cough of medicinal etiology)
It is estimated that approximately 15% of patients receiving any angiotensin-converting enzyme inhibitor (ACE) have chronic cough. The occurrence of cough does not depend on the ACE dosage. The timing of cough induction by ACEs is highly unpredictable, as it ranges from hours to one year after drug initiation34. Remission of cough after ACEs discontinuation usually happens 1–4 weeks later, with a mean time of 26 days, although longer periods (3 months to 40 weeks) have been reported35. Angiotensin II receptor antagonists are a safe substitute for ACEs in patients with chronic cough.
Sitagliptin, an antidiabetic DPP-4 inhibitor drug was wrongly considered as a cause for iatrogenic cough based on a publication of a series of 15 patients36. Although it has been associated with a slightly increased likelihood of nasopharyngitis, review of international literature has not confirmed its relationship with cough induction37.
Bisphosphonates and calcium channel antagonists can exacerbate pre-existing GERD, due to relaxation of the lower esophageal sphincter, and accordingly deteriorate chronic cough12. Eye drops containing prostaglandin analogues for the treatment of glaucoma (e.g. latanoprost) irritate the pharynx through the lacrimal duct and are also a potential cause of chronic coug38.
Chronic refractory cough
Chronic refractory cough (CRC) is defined as a cough that remains unexplained despite the extended diagnostic workup and persists despite guideline-based treatment. It is seen in 20–46% of patients presenting to specialist cough clinics and it has a substantial impact on quality of life and healthcare utilization12. Other terms that have been used to describe this clinical condition are unexplained chronic cough, idiopathic chronic cough, chronic refractory cough, or cough hypersensitivity syndrome (CHS)39. It is identified in about 20–46% of the patients who seek respiratory evaluation, and it has significant impact in life quality and use of health resources.
This neuropathic condition is often attributed to deregulation of neuronal pathways such as the transient receptor potential (TRP) receptors [transient receptor potentialvanilloid-1 (TRPV-1) and TRP ankyrin-1 (TRPA1)]. In some studies it is clearly associated with an increase of menopausal symptoms, depressive syndrome and autoimmune disorders40. Those patients often complain about pronounced sensitivity on environmental irritants such as perfume, bleach, and cold air, or during activities that are not supposed to provoke cough such as talking and laughing.
The diagnosis of CRC is not simple, as most common causes of cough must be ruled out before, following thorough evaluation and possibly treatment. The European Respiratory Society guidelines recommend the administration of neuromodulatory substances, mainly slow-release opioid–morphine formulations (in low dose, 5–10 mg twice daily), in adult patients with CRC (strong recommendation, moderate quality evidence)12. In a randomized double-blind placebo-controlled study where slow-release morphine sulfate was administered in patients with CRC, there was a similar improvement in cough between the 5 mg and 10 mg groups. Even in low doses, constipation and nausea were frequent undesirable side effects41. Similarly, the British Thoracic Society recommendations in 2022 focus on the fact that higher doses should be avoided, and in many cases once daily administration is sufficient.
Codeine formulations have been frequently administered to achieve an antitussive effect, but they cannot be used long-term due to their poor effectiveness and large variability of their metabolism in each patient42.
Pregabalin (a drug used for the treatment of epilepsy, neuropathic pain, fibromyalgia, restless legs syndrome and some anxiety disorders) has been used for CRC and showed benefit regarding the severity of cough and LCQ, but there was no significant difference in improvement in cough frequency between groups43. Initially, 25 mg twice daily (maximum dose of 75 mg twice daily) (BTS 2022) can be administered. Patients should be informed about adverse effects that require discontinuation of treatment, such as dizziness, weakness, ataxia and vision disturbances. These drugs should be avoided in patients that already receive central nervous system depressants and in patients with chronic respiratory diseases as they may suppress the respiratory center.
P2X3 receptor antagonists, with gefapixant being the main agent, have proved benefit for the treatment of CRC in phase II and III trials44. P2X3 receptors are adenosine triphosphate (ATP)-activated ion channels that are expressed on peripheral sensory neurons. Gefapixant is used in the dose of 45 mg twice daily, due to frequent side effects (dysgeusia, nausea, upper respiratory tract infection). A new P2X3 antagonist, camlipixant has shown significant benefit in the randomized face IIb trial SOOTHE, with satisfactory safety profile (data presented in ATS 2023).
Supplementary to drugs, non-pharmaceutical therapy, such as physiotherapy and speech pathology treatment, is also recommended for the treatment of CRC by ERS/BTS guidelines, with some proven benefits that lasted only for three months45. This kind of therapy can be supplementary to pharmacotherapy.