INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is characterized by persistent respiratory symptoms and airflow limitation and it is one of the main causes of morbimortality globally. Exacerbation is defined as a period of acute worsening of respiratory symptoms1. Exacerbations have a negative impact on patients’ everyday activities and quality of life2. There are three surgical options for severe COPD patients: bullectomy, lung volume reduction surgery and lung transplantation, and each surgical option has different eligibility criteria1. A pulmonary bulla is an air-filled space bigger than 1 cm in diameter and a giant bulla is defined as 1 or more bullae enlarged to occupy more than a third of the hemithorax3,4. Elective surgery is rarely performed due to the difficulty in predicting which patients will experience improvement in their symptoms and quality of life3. We present a case of a COPD male patient submitted to elective bullectomy.
CASE PRESENTATION
A 67-year-old man presented to the emergency department with progressively worsening shortness of breath and increased sputum production (yellow color). He did not report fever, wheezing, chest pain, weight loss, nausea, or vomiting. He quit smoking 30 years ago (30 pack-year smoking history). His past medical history included arterial hypertension, atrial fibrillation and COPD diagnosed 6 years ago, and a right pneumothorax 4 years ago that was treated with a chest drain. He used bilevel positive pressure airway (BiPAP) ventilator support and oxygen supplementation at home (long-term oxygen therapy and ambulatory oxygen therapy). Six months ago, he had a COPD exacerbation with similar symptoms which required hospitalization. Laboratory tests demonstrated leukocytosis and elevated C-reactive protein. The x-ray revealed a large bulla with air-fluid levels on the left hemithorax. The patient was admitted and empiric treatment with antibiotics was initiated, and was discharged home after 10 days with clinical and radiological improvement.
The baseline pulmonary function tests are listed in Table 1. The alfa-1-antitrypsin levels were normal. The six-minute walking test (6MWT) was interrupted at 211 meters because of important desaturation (minimum 76%) with oxygen therapy at 6 L/min. Our patient reported a modified British Medical Research Council (mMRC) grade 3 and a COPD Assessment Test (CAT) of 27.
Table 1
Pulmonary function tests
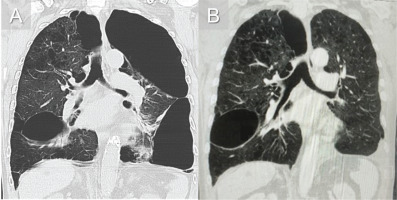
Chest computed tomography (CT) showed many large bullae with lung distortion, the largest of them being located in the apicoposterior segment of the left upper lobe with 204 mm (Figure 1A). There were no other significant findings. The patient was submitted to a bullectomy 4 months after the last COPD exacerbation. The post-operatory period was uneventful and the chest drain was removed 5 days after surgery, but his discharge was postponed due to a lack of social support. At outpatient revaluation six months after surgery, he was able to complete his daily tasks without oxygen therapy and without desaturation while walking. Our patient reported an mMRC grade 1–2 and a CAT of 11. The CT scan showed a reduction of areas with emphysema and the absence of the large bulla on the left (Figure 1B).
Figure 1
A) Coronal computed tomography image of large bullae showing an ipsilateral compressed lung; B) Coronal computed tomography image of the chest after left side bullectomy showing reexpansion of the compressed lung postoperatively
He did not perform a 6MWT at the follow-up at one year, but an arterial blood gas on room air showed pH7.40; partial pressure of carbon dioxide (pCO2) 44 mmHg; partial pressure of oxygen (pO2) 69 mmHg; bicarbonate (HCO3) 27 mmol/L; and peripheral saturation of 95%. The baseline and one year after bullectomy pulmonary function tests are listed in Table 1.
DISCUSSION
Bullae can be classified into three main types. Type I bullae arise above the pleural surface and are characterized by a narrow neck. Type II bullae arise from the subpleural parenchyma and are characterized by a broad neck. Type III bullae have no well-defined neck and are located deep in the lung3,5. There are several mechanisms related to the complex bullae pathophysiology. Progressive gas trapping will increase the bullae sizes, compress the surrounding lung parenchyma and compromise blood flow and ventilation, resulting in symptoms like dyspnea4,5.
Patient selection for bullectomy is a complex process. The goals of surgical treatment are to improve the quality of life and to relieve symptoms like dyspnea through the expansion of the remaining lung4. There are some favorable prognosis factors like localized disease, the presence of giant bullae, and FEV1 of less than half of the predicted value3. However, it has been hard to identify one preoperative test to predict which patients will benefit more from the surgical treatment, so the selection of patients is also based on the surgeon’s comfort and the experience of the center3,4. Marchetti et al.5 describe as an indication of bullectomy: the presence of compressed lung adjacent to bulla on CT scan; bulla occupying more than one-third of the hemithorax; and significant dyspnea that has not responded to aggressive medical therapy, like in our case. This surgical procedure is not free from complications, such as prolonged air leak, atrial fibrillation, pneumonia, or postoperative mechanical ventilation, so patient selection should take into account patients that have a higher risk such as active smokers or patients with previous cardiac disease5. Conflicting results have been reported about pulmonary function improvement after bullectomy with some studies questioning whether the improvement after bullectomy is or is not time-limited3,6,7. Schipper et al.7 demonstrated an improvement after 6 months post bullectomy in the 6MWT that disappeared after 3 years. In the same study, there was a permanent improvement at dyspnea and quality-of-life scores.
Our case suggests that symptoms in these patients could be a priority over pulmonary function. More than one year after surgery our patient maintains improvement in quality of life despite the persistent underlying emphysema and the small improvement in the overall pulmonary function tests. A multidisciplinary team is essential to accomplish appropriate care, complete preoperative evaluation, and postoperative management.
CONCLUSION
COPD is a worldwide growing problem and exacerbations have a key role in morbidity of these patients. Safety and cost-effectiveness analysis in surgery are essential, but selecting those patients who will benefit most from elective bullectomy is a challenging process, not only because the timing for treatment is not defined but also because there is a lack of literature on selection criteria for bullectomy. We believe that relief of symptoms in COPD patients should be a priority over pulmonary function, but larger studies are necessary to better understand the underlying variables that could be predictors of improvement in these patients. This will lead to better management of these patients and better surgical results.



