INTRODUCTION
Upper airway (UA) is anatomically the section of the airways that begins from the mouth opening and extends to the cricothyroid cartilage1. Upper airway obstruction (UAO) is a distinct condition that can arise from a group of heterogeneous causes. Clinically it can present with acute or chronic symptoms depending on the etiology and the dynamics of the luminal obstruction. Acute UAO is a medical emergency and the patient may present with stridor, gasping and cyanosis, and hypoxia2,3. It is a clinical diagnosis and warrants immediate airway management. A subacute or chronic presentation is usually in the form of progressive exertional dyspnea, hoarseness of voice, stridor, and cough. These conditions may be frequently misdiagnosed as other common differentials like chronic obstructive pulmonary disease (COPD) or asthma. In patients with acute UAO, a correct diagnosis is critical, as the definitive therapy often requires surgery. Once diagnosed and treated appropriately, the results are gratifying with complete resolution of symptoms. UAO can further be classified as variable if the severity of obstruction varies according to phase of respiration or fixed where the severity of obstruction is unaltered irrespective of the phase of respiration2. UAO can further be classified as variable extrathoracic UAO (VET UAO) or variable intrathoracic UAO (VIT UAO), depending on the location of the obstruction. Definitive diagnosis of UAO requires the inspection of UA by invasive maneuvers laryngoscopy or bronchoscopy.
Another simple bedside test which gives us a lucid idea about the presence of UAO is spirometry with its flow volume loop (FVL). Spirometry is the most commonly employed pulmonary function test (PFT) which basically measures the volume and speed of air exhaled and inhaled. While radio-imaging is ideal, in remote areas or critical cases a bedside test is more useful to diagnose the site of lesion. By these virtues it becomes an ideal screening test in cases of suspected UAO. Recording a FVL is a vital and integral component of spirometry. The countenances of the FVL not only help us in determining the presence of UAO but also help us in gauging the site (intrathoracic or extrathoracic) and the nature (fixed or variable) of the obstruction3,4. Hence, not only the visual appearance of the FVL (flow volume envelope) but the upper airway indices should be taken into consideration4. The symptoms in UAO appear when the obstruction is relatively severe. However, a FVL may show aberrations much before these symptoms manifest2. Hence, if a high index of suspicion is maintained, FVLs help in the early detection of UAO before symptoms manifest. Despite this broad attention to the diagnostic value of the FVL, there is a dearth of studies to correlate FVL features with various other diagnostic techniques. These gaps are specifically pertaining to the prevalence of UAO, the availability of visual and quantitative criteria, and their ability to detect UAO. Hence this study was conducted with the aim to address these questions.
METHODS
This study was conducted in the department of pulmonary medicine in a tertiary care hospital attached to a public medical school, after institutional ethics committee approval. It was a retrospective study with the intention of studying the role of spirometry with FVL in a case of UAO. The objectives were to study the prevalence of UAO, to calculate the sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the individual criteria of FVL for predicting UAO and to study the ability of spirometry with FVL to differentiate between VET UAO and VIT UAO. The data set included consecutive spirometries performed at the pulmonary function laboratory in our center from January 2011 to December 2013. Patients who had incomplete clinical data and diagnostic workup were excluded from the study. The accepted standard tests for diagnosing UAO are bronchoscopy, laryngoscopy, and chest or neck computed tomogram (CT). A patient record was included only if the patient had both an evaluable spirometry and one of the aforementioned imaging or endoscopic upper airway examinations.
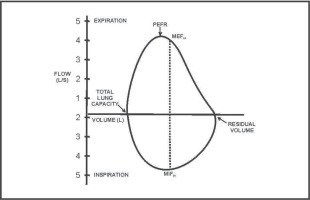
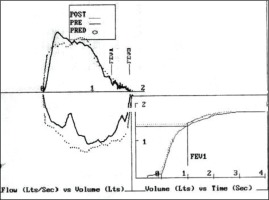
A spirometer consisting of a dry pneumotachograph (Medgraphics Profiler DX Pulmonary Diagnostic system) which complied with the ATS criteria was used5. During spirometry, the subject inhaled to total lung capacity (TLC) and then exhaled forcefully to residual volume (RV) followed by rapid inhalation to TLC again. A maximum of eight efforts were allowed to ensure adherence to ATS spirometry guidelines; otherwise, the test was abandoned and the patient was given a reappointment. A flow transducer produced an electric signal, which was computed by a microprocessor, displayed on the screen and recorded. The flow was plotted on the y-axis and the volume on the x-axis to construct an FVL. A normal FVL shows diminished flow as the lung volume shrinks, seen as slight coving near the RV on the expiratory curve. This occurs due to compressive forces during exhalation and distension by negative pressures during inhalation. The criteria recommended by the American Thoracic Society were used to select the best test of a minimum of three respiratory maneuvers5. The included spirometries were all studied for indices of UAO to determine the role of different indices. The proportion of patients with UAO was noted. All studies were analyzed for two quantitative and one qualitative UAO indices to determine the presence of UAO. The differentiation of UAO into fixed, VET UAO and VIT UAO was done. For UAO, qualitative analysis of the FVL in form of visual inspection of the FVL with respect to flattening of the inspiratory/expiratory portions, a box shaped loop or oscillations were used as the criteria. The FVLs were assessed by a senior resident doctor of pulmonology and studies diagnostic of UAO were confirmed by a senior professor.
For quantitative analysis, two ratios were calculated. The first one was Empey’s index6. It is the ratio of forced expiratory volume in 1 second (FEV1) and peak expiratory flow (PEF). An Empey’s index greater than 10 mL/L/min suggests presence of UAO. The second index was forced inspiratory flow at 50% of the vital capacity (FIF50) ≤100 L/min7. A ratio of the maximum expiratory to inspiratory flow at 50% of forced vital capacity (FEF50/FIF50) was also calculated to differentiate the type of UAO into VET UAO or VIT UAO. FEF50/FIF50 >1 indicates variable extrathoracic VET UAO, whereas FEF50/FIF50 <0.3 indicates variable intrathoracic VI UAO8. We calculated the sensitivity, specificity, PPV and NPV of the individual criteria. Continuous variables were reported as mean with standard deviation (SD), and percentiles. Categorical variables were reported as frequencies and percentages. The data were statistically analyzed to determine the prevalence of UAO in the study group and the sensitivity, specificity, PPV and NPV values of the individual criteria of FVL for predicting UAO were calculated.
RESULTS
Spirometry records of 986 patients were available in the study period. Of these, 772 spirometries with FVL and complete diagnostic workup were included in the study. In all, 214 studies were excluded in view of incomplete clinical details. The mean age of the population was 43 years. Most common diagnoses were COPD, BA, post infectious obliterative bronchiolitis, and interstitial lung disease (ILD). Twenty-four patients demonstrated UAO in clinicoradiological and spirometry correlation. Hence, the proportion of UAO amongst the total patients performing spirometry was 3.1%. The most common cause of UAO in our study was multinodular goiter (MNG) seen in 10 (39%) of our patients. The other causes were vocal cord dysfunction (VCD) in 4 (18%), post intubation tracheal stenosis (PITS) in 3 (13%), Lingular tonsils and tracheal masses in 2 patients each (9%), while obstructive sleep apnea (OSA), tracheitis and Arthrogryposis multiplex congenita (AMC) in 1 patient each (4%).
Analysis of Empey’s index revealed that the average value was 5.62 (2.56) mL/L/min in the total spirometries performed while in patients with UAO, the average value was 8.70 (3.59) mL/L/min. The sensitivity, specificity, PPV and NPV for Empey’s Index were 62.5%, 89.4%, 15.7% and 98.6%, respectively. A visual examination of the FVL revealed FVL abnormalities in the form of flattening of either loop, box-shaped loops, and saw tooth pattern; compare Figure 1 (normal) with Figure 2 (abnormal) (further abnormal examples are given in Supplementary file Figures S1 to S3). The sensitivity, specificity, PPV and NPV, for these qualitative criteria of examination of FVL, were 95.6%, 99.7%, 91.6% and 99.8%, respectively. Analysis of the FIF50 <100 L/min parameter revealed that sensitivity, specificity, PPV and NPV, of these criteria for detection of UAO, were 79.1%, 80.4%, 11.5% and 99.1%, respectively (Table 1). The combined analysis of the quantitative and qualitative criteria was able to correctly predict the location of UAO in all cases (100%). In our study, out of the 24 patients, 17 were cases of VET UAO, 4 were VIT UAO while 3 cases had fixed UAO. The FEF50/FIF50 ratio was able to differentiate correctly the type of UAO as VET UAO /VIT UAO/fixed UAO in 20 out of the total 24 cases. In 86.95% of patients of UAO, the location of obstruction was predicted accurately by indices and in 95% with use of FVL.
Table 1
The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of the Empey’s index, visual examination of the flow volume loop and the FIF50 <100 L/min in the diagnosis of upper airway obstruction (UAO)
| UAO index | Sensitivity % | Specificity % | PPV % | NPV % |
|---|---|---|---|---|
| Empey’s index | 62.5 | 89.4 | 15.7 | 98.6 |
| Flow volume loop | 95.6 | 99.7 | 91.6 | 99.8 |
| FIF50 <100 L/min | 79.1 | 80.4 | 11.5 | 99.1 |
DISCUSSION
UAO is a frequently neglected entity and can cause morbid implications. This study was conducted in the pulmonary medicine department of our tertiary care hospital with the endeavor to study the prevalence and profile of UAO and to analyze the utility of various FVL indices in the diagnosis of UAO. The prevalence of UAO in patients who underwent spirometry for various reasons in the PFT laboratory of this pulmonary medicine department was 3.1%. An earlier study of consecutive spirometry by Modrykamien et al.1 reported a prevalence of 7.5%. The lower prevalence of UAO could be attributed to the fact that, ours being a dedicated pulmonary unit, some cases were missed as they would be likely consulting an otorhinolaryngology clinic. The analysis of the etiological profile of the UAO in our study group revealed that the most common cause of UAO was MNG, seen in 39% of our patients. The other common causes were VCD and PITS. This is in contrast to the study done by Modrykamien et al.1 where the most common causes were tracheal granulation and dynamic tracheal collapse. A huge number of patients in our country, particularly females, develop goiters which seem to be indolent. However, if not detected early, they can cause significant symptoms and airway compromise; FVL is a simple and non-invasive method of assessing the UAO in these patients. They can even uncover abnormal airflow dynamics even in asymptomatic goiters aiding an early evaluation and timely surgery9. Another common cause for UAO in this study was VCD. This is a frequently neglected entity which occurs due to upper airway neural instability10. It is habitually misdiagnosed as asthma which is difficult to control10. FVL with indices frequently reveals the UAO10 with predominant VET UAO pattern of flattening of the inspiratory loop11. PITS is a common cause for UAO and is inadequately studied12. PITS can occur as sequelae in 10–22% of invasive endotracheal intubation cases due to the physical injury to the tracheal mucosa with the resultant inflammatory cascade. The symptoms, in the form of exertional dyspnea and cough, emerge only after a significant luminal compromise and can lead to delay in seeking medical care. Spirometry with FVL exhibits features of UAO even before the clinical manifestations and hence aids in early diagnosis and management12.
FVL are particularly important in obstructive sleep apnea (OSA), as it is a simple and inexpensive objective method to predict the presence and the severity of UAO. The saw-tooth sign on FVL in OSA was first described by Sanders et al.13 in patients with OSA. It is hallmarked by the presence of three or more consecutive peaks and troughs occurring at regular intervals. The underlying mechanism has been attributed to turbulent flow due to sporadic narrowing of the upper airway due to the tissue redundance. However, saw toothing can be observed in other conditions like neurological disorders too. In a study by Ashraf et al.14, a saw tooth sign was present in 26.1% of the patients with OSA, however it did not correlate with the apnea hypoapnea index (AHI)14. In this study, two patients of OSA showed spirometry FVL changes of UAO. FVL showed inspiratory loop flattening in one patient while another patient had saw toothing of loops. Patients with OSA need to be triaged as per the clinical severity and the pretest probability scores so that those that need a polysomnography (PSG) on priority get an opportunity to be tested at the earliest. This clinical determination of the pretest probability is further supported by evidence of an UAO on FVL. Since this was a study on the prevalence of UAO centered at a pulmonology department catering for infectious respiratory diseases, cancer, and chronic respiratory disease, the overall cases of OSA with UAO was less.
Analysis of Empey’s index, gave the sensitivity, specificity, PPV and NPV as 62.5%, 89.4%, 15.7% and 98.6%, respectively. Empey’s index, though widely recognized, was found to be the least sensitive in our study. In the original study done by Empey, which compared the index between 10 normal subjects and 18 patients with UAO, this index was significant in all of the UAO cases and in none in the cases without UAO. However, his study included patients with severe UAO which presented with evident stridor on their clinical examination6. In the study done by Hira et al.7, Empey’s index was altered significantly (p<0.001) and the cut-off value used was above 10 mL/L/min. This emerged as the second best to recognize UAO after the FEF50/FIF50 ratio.
A visual examination of the FVL revealed abnormalities in the form of flattening of either loops or box-shaped loops. The sensitivity, specificity, PPV and NPV for these qualitative criteria of examination of FVL were 95.6%, 99.7%, 91.6% and 99.8%, respectively. Flow volume loop analysis in this study showed higher sensitivity compared with previous studies1,7. Retrospective study with interpreter not being blinded to the diagnosis may have added to the increased sensitivity of qualitative criteria in our study. Analysis of the FIF50 <100 L/min parameter revealed that sensitivity, specificity, PPV and NPV of the criteria for detection of UAO were 79.1%, 80.4%, 11.5% and 99.1%, respectively. This is consistent with the findings reported by Hira e al.7. The FEF50/FIF50 ratio was able to differentiate the type of UAO into VET UAO and VIT UAO in 20 out of the total 24 cases. In the study done by Hira et al.7, it was observed that a FEF50/FIF 50 ratio >1 proved to be the most superior indicator for fixed and variable extrathoracic UAO.
Strengths and limitations
In this study, all the tested diagnostic criteria for detecting UAO showed a sensitivity ranging from 62.5–95.6%, which is considerably higher in comparison with earlier studies1. Again, the investigator not being blinded to the diagnosis of UAO could have contributed a certain level of bias, especially for the qualitative criteria. Among the indices, the high negative predictive value of Empey’s index (98.6%) requires greater attention for its role in excluding an upper airway obstruction. The correlation between the extent of obstruction and value of Empey’s index has been poor and non-uniformity of evaluation in cases of UAO restricts further comments on this topic based on this study. Though FVL too has a high negative predictive value (99.8%), qualitative variables are observer-dependent and may have less application than Empey’s index in this matter. FIF50 <100 L/min as an index showed considerable sensitivity and negative predictive value, but high false positive rates make it less reliable unless combined with other indices. FVL is also subject to limitation of patient performances leading to a poorer sensitivity, particularly in the pediatric age group or in patients with acute sign limiting their ability to perform15,16. These overall characteristics of the FVL and the indices reiterate that although these indices are deficiently sensitive for detection of UAO, they can be used as a screening tool for UAO in the correct clinical context. A normal FVL morphology and a normal index value may not be able to exclude the presence of UAO, but a positive FVL quantitative and qualitative trait definitely helps us to select patients with UAO. Also, FVL characteristics and indices help to differentiate the type of UAO in the majority of patients, and hence can guide the further invasive endoscopic or imaging approach.
CONCLUSIONS
UAO is a common but perfunctorily fathomed entity. Spirometry with FVL is an excellent screening tool for UAO by virtue of its simplicity, ease of availability, and non-invasiveness. A timely index of suspicion and performance of a spirometry with FVL in the appropriate clinical context can aid in the early diagnosis of UAO. There are very few studies done on a large sample in a tertiary care hospital to find the prevalence and etiological pattern of UAO and also attempts to decipher the utility of various FVL indices. The limitations of this study were that being a retrospective analysis we had a restricted number of patients included in our study. No blinding of investigators may have influenced the interpretation of qualitative variables. Also, since it was not a community-based study, the extrapolation of prevalence of UAO and related characteristics were subject to referral bias.