INTRODUCTION
Melioidosis is a clinical disease caused by B. pseudomallei, which is endemic in South-East Asia and Northern Australia. The infection is usually acquired through percutaneous inoculation or inhalation of the bacterium present in soil and surface water in the endemic region1. Risk factors for melioidosis include diabetes, alcoholism, and chronic renal disease, which are associated with increased mortality.
Melioidosis is a great mimicker of many clinical conditions and commonly presents as community-acquired pneumonia (CAP), which is very worrying, as melioidosis present with pneumonia is associated with a high mortality rate2. At least 10% of cases present with a chronic respiratory illness, mimicking tuberculosis and often with upper lobe infiltrates and/or cavities on chest radiography3.
The proper data on incidence of lower respiratory tract infections are not available in India. But as per the WHO report, the mortality rate due to lower respiratory tract infections in individuals aged >65 years is 6.2 per 1000 deaths4. Melioidosis is still a rare disease in India where the incidence of CAP and pulmonary tuberculosis is very high. Since CAP and pulmonary tuberculosis are common conditions managed in primary care settings, it is imperative for doctors to understand the clinical presentation of melioidosis with pulmonary involvement.
Timely diagnosis of melioidosis is crucial in preventing mortality. Hence, we report a rare case of melioidosis that presented clinically and radiologically as community-acquired pneumonia. Timely diagnosis and treatment helped in complete recovery of the patient.
CASE PRESENTATION
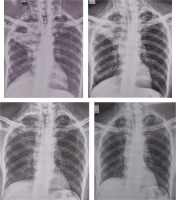
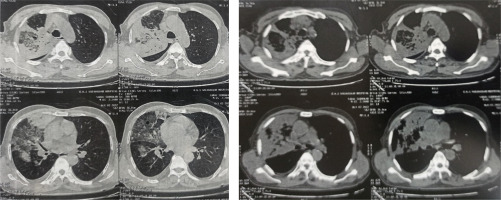
A 65-year-old farmer from a coastal region of India, who was a known diabetic, presented with a high-grade intermittent fever associated with chills, cough with purulent expectoration, and right-sided dull aching chest pain for 2 weeks. Chest X-ray showed a cavitary consolidation in the right upper lobe. A provisional diagnosis of community acquired pneumonia and pulmonary tuberculosis was made. The patient was started on beta lactams and macrolides. To rule out pulmonary tuberculosis, sputum GeneXpert was done and MTb was not detected.
Despite receiving empiric antibiotics as per the guidelines, the patient had persistent fever and a few episodes of mild hemoptysis. Total leukocyte count was 16560/mm3, and procalcitonin was 1.1. In view of persistent fever, increased leukocyte count and raised procalcitonin, antibiotics were stepped up to iv piperacillin-tazobactam and iv amikacin.
Sputum Culture showed B. pseudomallei, sensitive to piperacillin-tazobactam, cefoperazone-sulbactam, amikacin, ceftriaxone, meropenem, levofloxacin, and resistant to ceftazidime, minocycline, amoxycillin/clavulanic acid and, gentamycin. Blood culture was negative. Ultrasound of abdomen was normal. Clinical and laboratory results gave a diagnosis of pulmonary melioidosis with no other organ involvement.
As culture was sensitive to the antibiotics, the patient was treated with iv piperacillin-tazobactam and iv amikacin for 14 days. Then, the patient was started on oral trimethoprim/sulfamethoxazole and doxycycline as per guidelines5. Symptomatic and radiological improvement was seen within 1 week of starting treatment. Bronchoscopy was done after 2 months to confirm eradication of the bacterium, and sputum gram stain and aerobic culture showed no growth. Trimethoprim/sulfamethoxazole and doxycycline were continued for 3 months. Complete clinical improvement and almost complete radiological resolution were seen.
DISCUSSION
Melioidosis is a clinical disease caused by B. pseudomallei. It is a facultative, intracellular, saprophytic, gram-negative organism widely present in soil and surface water. Individuals at risk are those who are exposed to wet soil or surface water like farming, agriculture, gardening and fishing6. The portal of entry for the bacterium is direct inoculation from damaged skin or inhalation. It is endemic to tropical regions of South-East Asia, Asia and subtropical areas of Australia. In India, most of the cases were reported from the coastal region, though melioidosis may be more widely prevalent7.
Diabetes mellitus, alcoholism and chronic renal disease are the identified comorbidities which are the risk factors in the majority of melioidosis cases and are associated with increased mortality. DM has been found to be one of the most frequent predisposing factors. One study from India found a 76% correlation of diabetes with melioidosis8.
Melioidosis can have 2 major presentations; acute infection (symptoms lasting <2 months) and chronic infections (symptoms lasting >2 months). Melioidosis can present as septicemia, localized infection with/without abscesses and ulcers, asymptomatic infections, pneumonia, visceral abscesses, neurologic infection, and musculoskeletal infections. Melioidosis is a systemic disease with pulmonary involvement being the commonest manifestation. It is also associated with liver and spleen related manifestation6,7.
Pulmonary melioidosis presents with symptoms of cough, fever, chest pain, and headache. Disseminated infection presents with weight loss, abdominal pain, muscle and joint pain, and seizures etc.5,9.
The standard method for diagnosing melioidosis is the isolation of B. pseudomallei from clinical specimens using culture. However, this bacterium if often misidentified as a species of Pseudomonas, which can lead to misinterpretation of the disease as hospital-acquired and underestimation of its true incidence. Most patients with melioidosis exhibit clinical and radiological symptoms of pneumonia, and commonly use antipseudomonal antibiotics like meropenem, ceftazidime, levofloxacin, and amikacin, which can be effective against B. pseudomallei. More sensitive diagnostic tests are available, such as PCR-based methods and rapid identification technologies like gene sequencing and matrix-assisted laser desorption ionization time of flight mass spectrometry (MALDI-TOF MS)10.
CONCLUSION
The treatment of melioidosis is prolonged, and includes 2 phases: intensive treatment with intravenous antimicrobial therapy for 10–14 days and eradication phase with oral antibiotics. Meropenem and ceftazidime have shown to be effective in acute stages. At least a 10-day intravenous therapy is recommended. In a study, 4% of infected patients who were treated with intravenous antibiotics had a relapse of infection due to the persistence of the organism in the body. In a study from Thailand, relapse rate was 9.7% and it was not associated with duration of intensive treatment9. Hence, an eradication phase with oral antimicrobial therapy for 3–6 months with trimethoprim/sulfamethoxazole is recommended. Doxycycline is used as second line drug if trimethoprim/sulfamethoxazole cannot be used or is not tolerated5.