INTRODUCTION
Lipoid pneumonia refers to pneumonia due to inhalation or aspiration of lipid-rich chemical products and is well documented with diesel ingestion1.
Patients present with wide range of symptoms like cough, shortness of breath, less commonly with hemoptysis and fever, often mimicking other lung conditions such as malignancy.
CT findings typically include appearances of consolidation, usually involving bilateral lung fields with either segmental or lobar distribution and predominantly involving the lower lobes followed by middle lobes of lung. Crazy paving pattern can also be visualized. Pneumothorax and pneumomediastinum are rare presentations, but can occur early in disease2,3.
Baron et al.4 studied radiological and clinical findings of acute and chronic exogenous lipoid pneumonia and they found masses in 4 out of 6 patients with chronic and in none of the patients with acute presentation.
CASE PRESENTATION
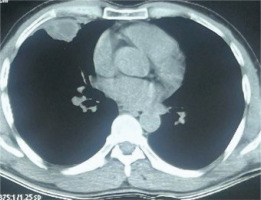
A 65-year-old male smoker presented with a history of fever, cough, and right-sided chest pain which worsened on coughing and deep breathing, and single episode of blood streaking of sputum for 6 days. He visited a local practitioner for the above complaints and underwent a chest X-ray which showed homogenous opacity in the right mid-lung zone. He was further investigated and underwent a contrast enhanced computed tomography scan which was suggestive of a heterogenous and peripheral enhancing necrotic mass of approximately 28/54/49 mm (anteroposterior/transverse/craniocaudal) size which was seen in the medial segment of the right middle lobe abutting the cardiac border medially and chest wall anteriorly without invasion, along with diffuse ground glass haze with septal thickening in the adjacent right middle lobe. Also, enlarged sub-centimetric mediastinal lymph nodes were noted (Figure 1). These findings favored a malignant nature of lesion over an infective etiology for which the patient was further evaluated.
Figure 1
Contrast-enhanced CT scan showing heterogenous and peripheral enhancing necrotic mass in the medial segment of the right middle lobe
During his evaluation, detailed history was obtained where the patient revealed that his symptoms occurred acutely following accidental ingestion of diesel while working at the farm. Following this, a differential diagnosis of lipoid pneumonia was considered and IV antibiotic, hydrocortisone and analgesics were started.
Further, to rule out the possibility of malignancy transthoracic CT guided fine needle aspiration cytology (FNAC) was performed and the cytological examination of the sample showed benign endobronchial cells with reactive and hyperplastic changes including a fair number of inflammatory cells along with foam cells, few reactive giant cells, and granulation tissue. No feature suggestive of malignancy could be seen on Papanicolaou staining of samples (Figures 2 and 3). ZN stain for AFB, and KOH stain for fungi, were negative. Background was mucoproteinaceous. Henceforth, the above findings confirmed our diagnosis of lipoid pneumonia.
Figure 2
The smear shows inflammatory cells with foam cells on transthoracic CT-guided FNAC (20×, MGG)
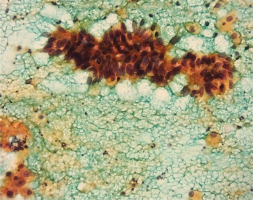
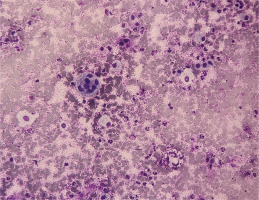
Figure 3
The smear shows hyperplastic and reactive epithelium on FNAC. Negative for malignant cells (40×, Papanicolaou stain)
The patient showed improvement in two days following initiation of therapy and was then discharged within a week’s duration. On follow-up after 10 days of initial presentation, the patient remained asymptomatic and chest X-ray showed complete resolution of the lesion.
DISCUSSION
In contrast to reported radiological findings1-4, our case is atypical as acute in onset, lesion being well defined round to oval peripheral enhancing mass on CT scan which was confirmed on cytology examination. Nakagawara et al.5 reported positron emission tomography (PET) scan finding of a histopathological confirmed case of lipoid pneumonia. The FDG uptake was distributed in spots in the area of consolidation, standardized uptake value (SUV) of 5.7 and partly matched with the fat-density areas on corresponding CT5. Cheng et al.6 also reported a PET scan finding of a case of lipoid pneumonia with FDG uptake, notably strong at the center of the fatty lesion. We did not perform a PET scan because of affordability issues of the patient.
Symptomatic management is the mainstay of treatment with reservation of antibiotic therapy in patients with superadded infection. Role of corticosteroids depends on presentation, severity and condition of the patient, although not well defined. Steroids can specially be effective in cases with presence of dense inflammation, as demonstrated on FNAC in our case. We managed our patient with intravenous hydrocortisone with antibiotic coverage which led to significant improvement soon after initiation of therapy.
CONCLUSION
We hope our case will add knowledge in the existing literature related to radiological findings and management of the disease. Due to the rare occurrence of the disease, a high index of suspicion and careful history, specially related to exposure, are needed for diagnosis of lipoid pneumonia. Cytology examination and steroids may be helpful in diagnosis and treatment respectively, and should be used on case-to-case basis.