Endobronchial lipoma is a rare benign tumor, with an estimated prevalence of 0.1–0.5% of all tumours1. This histological variant is typically found in subcutaneous tissue and has a low incidence in pulmonary tissue2.
A 56-year-old male patient, a non-smoker, presented to the Emergency Department with fever and a productive cough. Pneumonia in the left lower lobe (LLL) was suspected, and he was treated with antibiotics, showing clinical improvement. However, due to persistent radiological abnormalities, a chest CT scan was performed, revealing an endobronchial lesion with fatty density (−125 to −109 HU), approximately 1.7 cm in length, protruding into the lumen of the LLL bronchus and extending to bronchi B7 and B8 and their subsegmental branches (Figures 1A and 1B). Further investigation was initiated to exclude pulmonary neoplasia. A flexible bronchoscopy (FB)3 identified a bilobed, pedunculated endobronchial mass in the LLL bronchus, with a smooth pink surface and an appearance suggestive of a benign or intermediate malignancy obstructing B8 (Figures 2A and 2B). A bronchial biopsy was taken.
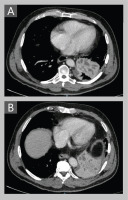
Figure 1
Coronal (A) and transverse (B) CT scans of the chest showing an endobronchial lesion of fat density (-125 to -109 HU) located in B7 and B8, with associated atelectasis at that level. In the upper right corner of (B), an enlarged image of the lesion, situated in the center of the image, is displayed

Figure 2
Flexible bronchoscopy image showing an endobronchial mass in the left lower lobar bronchus, bilobulated, pedunculated, with smooth pink surface causing B8 obstruction (A and B). Remnants of the lesion after partial resection by diathermine loop and YAG laser (C), with outflow of pus (C and D)
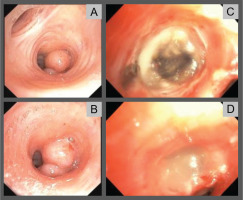
One week later, the patient returned with fever, left-sided pleuritic pain, and elevated inflammatory markers (C-reactive protein 447 mg/L, procalcitonin 1.34 ng/mL). A new CT scan revealed dilation and fluid density within the subsegmental branches of B8, alongside a mild pleural effusion, consistent with post-obstructive pneumonia (Figures 3A and 3B). The patient was admitted, and the biopsy confirmed the presence of mature adipose tissue, diagnosing an endobronchial lipoma. The lesion was resected via FB, coagulated, and partially excised using a diathermy loop, clearing the bronchus (Figure 2C). The tumor originated from B8, where it had a sessile base that was severed with the loop. Subsequently, a YAG laser at 15W was applied, but no vaporization occurred. Significant pus drainage was observed (Figure 2D). The patient was referred to Thoracic Surgery, where an initial attempt at video-assisted thoracoscopic lobectomy was converted to a lateral thoracotomy due to adhesions.
Figure 3
Cross-sectional slices of the CT scan performed 10 days after the initial CT scan (as shown Figure 1), showing a pseudomass image due to dilation and fluid density occupying the subsegmental branches of B8
The diagnosis of endobronchial lipoma can be delayed or mistaken for other conditions such as pneumonia or obstructive pulmonary diseases2. It is more common in males between the fifth and seventh decades of life. The majority of cases are on the right side and within the first three bronchial subdivisions1. Symptoms depend on the lesion’s location, degree of bronchial obstruction, and the resulting effects on the distal parenchyma, with common symptoms including dyspnea (40%), expectoration (30.6%), and persistent cough (27.8%)4. Chest CT is highly specific and sensitive for detecting adipose tissue within the lesion (−100 HU). Differential diagnosis through imaging should consider other pathologies such as bronchial carcinoid tumor (which is typically an intraluminal mass but lacks fat density) or hamartoma (which may also exhibit fat density but is often associated with calcifications)5. FB should differentiate it from bronchogenic carcinoma (which usually has an irregular surface), inflammatory polyps, carcinoid tumor, and granulomas (which present a more friable surface)6. FB is crucial for diagnosis, and endoscopic resection is the first-line treatment, with various endobronchial techniques available (YAG laser, cryotherapy, etc.)1,7. In cases where these interventions fail, surgical resection is considered.



